INFECTIVE ENDOCARDITIS
(IE)
-
DEFINITIONS
-
DIAGNOSIS
-
IMAGING
-
INDICATION AND TIMING OF SURGERY
<
>
Endocarditis:
Infective Endocarditis:
- Exudative and proliferative inflammatory alterations of the endocardium, characterized by vegetations on the endocardial surface or within the endocardium.
- It may occur as a primary disorder (infective endocarditis) or as a complication of or in association with another disease (e.g., lupus erythematosus, rheumatic heart disease).
Infective Endocarditis:
- Invasion and multiplication of microorganisms:
- On the endocardial surface.
- Within the endocardium.
- Within the myocardium
- On prosthetic materials.
- Within and around cardiac structures.
- Includes conditions in which structures of the heart, most frequently the valves, harbour an infective process that lead to:
- Valvular dysfunction.
- Localized or generalized sepsis.
- Sites for embolism.
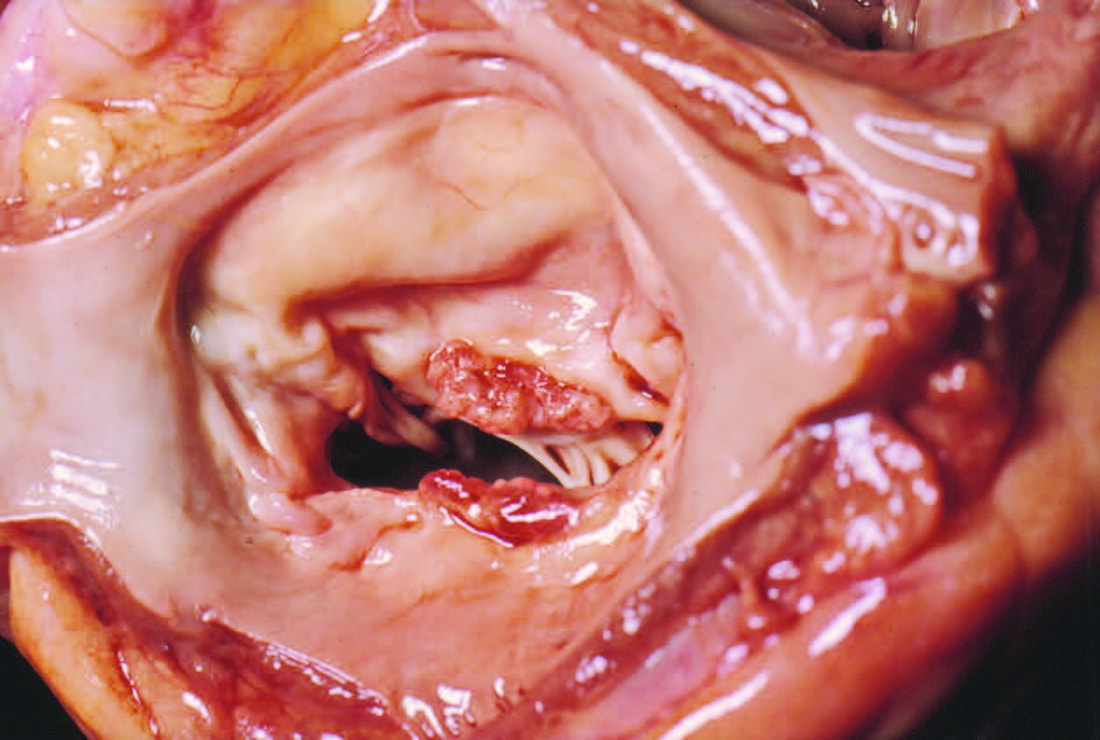
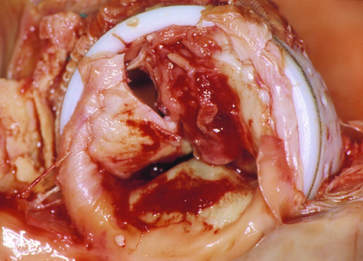
Native Mitral Valve Endocarditis with Vegetation on Both Leaflets
MODIFIED DUKE CRITERIA FOR THE DIAGNOSIS OF IE
MAJOR CRITERIA |
Positive Blood Culture |
Typical microorganisms for IE from two separate BC (in absence of primary focus)
|
OR |
Persistently positive BC (recovery of microorganism consistent with IE from:
|
Evidence of Endocardial Involvement: |
Positive Echocardiogram for IE: Oscillating intracardiac mass (in the absence of an alternative anatomic explanation)
|
OR |
|
HACEK Group:
- Haemophilus
- Actinobacillus
- Cardiobacterium
- Eikenella
- Kingella
MINOR CRITERIA |
Predisposition:
|
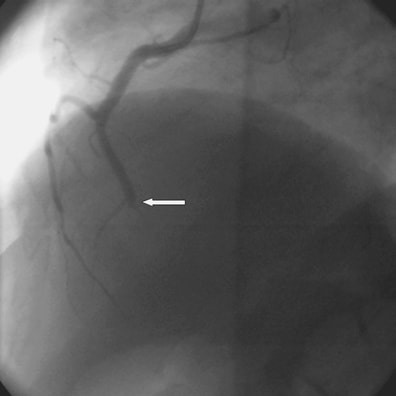
Vascular Phenomena:
|
Immunologic Phenomena:
|
Microbiological Evidence:
|
Echocardiography:
|
Definitive Diagnosis |
Two Major Criteria One Major + Three Minor Criteria Five Major Criteria |
Possible Diagnosis |
One Major + One Minor Criteria Three Minor Criteria |
Echocardiography:
- Echocardiography Is the imaging of choice for all cases with clinical suspicion of endocarditis.
- Echocardiogram should be repeated weekley if the first TOE study was not conclusive.
IE: Echocardiographic and Clinical Features Suggesting Potential Need for Surgery |
Vegetations:
|
Valvular Dysfunction:
|
Perivalvular Extension:
|
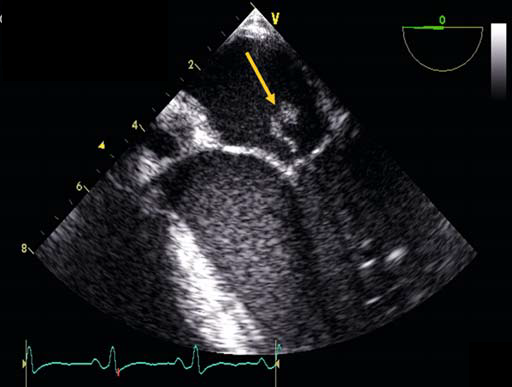
TOE showing multiple vegetations on the Aortic valve
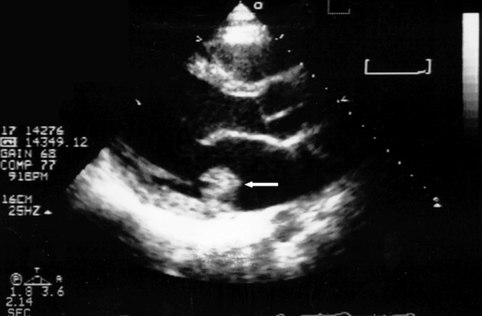
TTE showing large vegetation on posterior leaflet of MV (arrow)
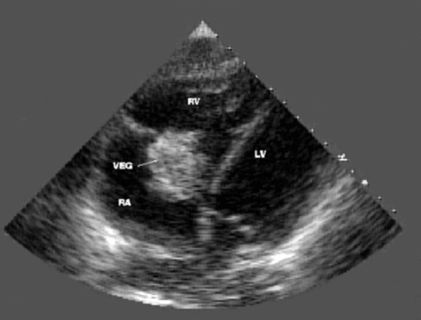
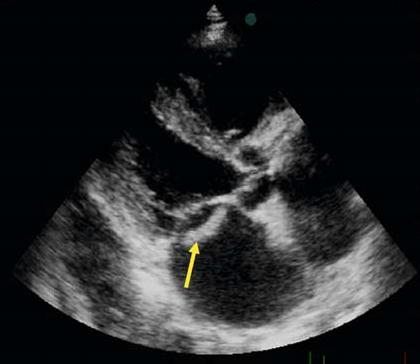
TTE showing large (4 cm diameter) vegetation (VEG) on the tricuspid valve in an IV drug abuser
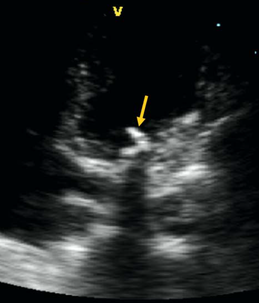
Apical 4-chamber view of TTE showing a large, mobile, lobulated vegetation (arrow) partially obstructing the tricuspid valve and prolapsing into the right ventricle
TOE showing vegetations on the MV
Complications of IE
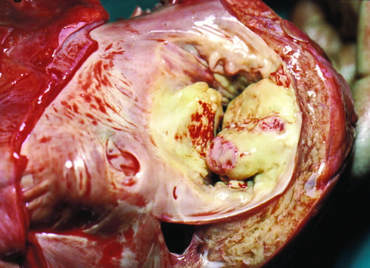
Partial Detachment of a Mitral Prosthetic Annuloplasty Ring due to Suture Dehiscence.
(separation between the mitral annulus and the prosthetic ring).
(separation between the mitral annulus and the prosthetic ring).
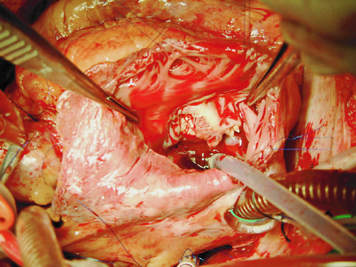
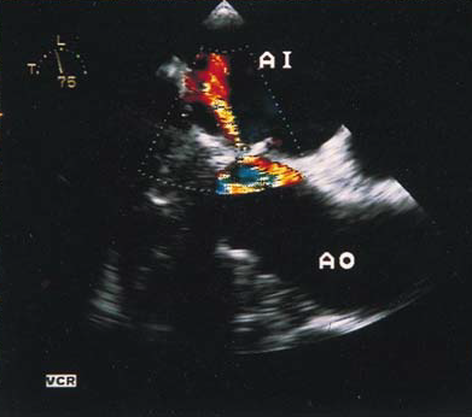
IE of the AV showing severe AR and an aneurysm of the Sinus of Valsalva
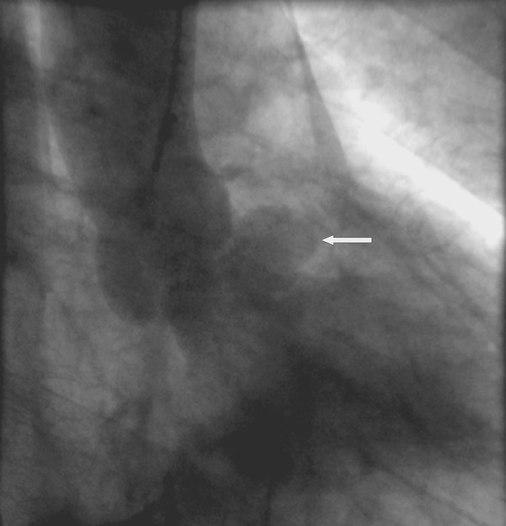
TOE showing a fistula between the aorta and the left atrium
in a patient with a mechanical aortic prosthesis
in a patient with a mechanical aortic prosthesis
IE: INDICATIONS FOR SURGERY |
Congestive Heart Failure:
|
Periannular Extension:
|
Systemic Embolism:
|
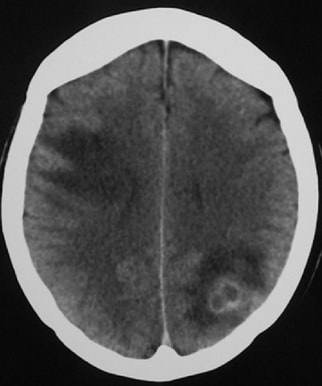
Cerebrovascular Complications
|
Persistent Sepsis:
|
Difficult Organisms:
|
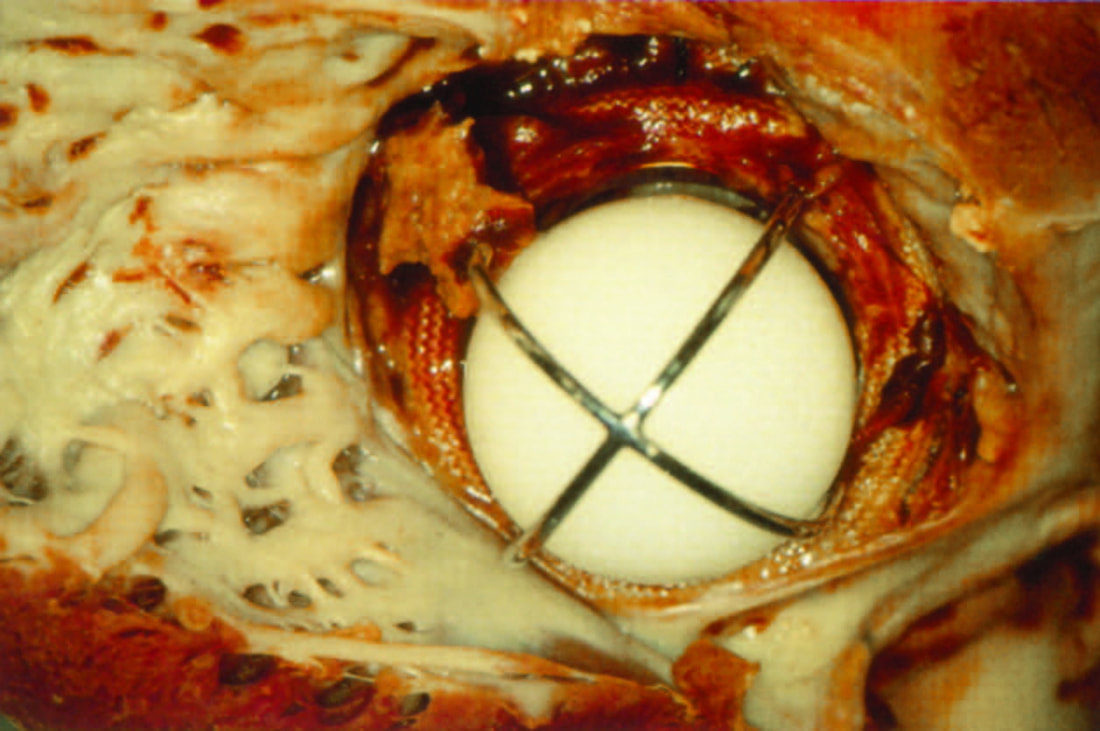
Prosthetic Valve Endocarditis:
|
IE: TIMING OF SURGERY |
Emergency Surgery (Within 24 Hours): NVE or PVE and severe CHF or cardiogenic shock caused by:
|
Urgent Surgery (Within Days):
|
Early Elective Surgery (During In-Hospital Stay):
|
SUMMARY
Indications and Timing
Indications and Timing
INDICATION |
TIMING |
CLASS |
LEVEL |
Heart Failure Aortic or Mitral NVE or PVE with severe acute regurgitation or valve obstruction or fistula causing refractory pulmonary edema or cardiogenic shock |
Emergency |
I |
B |
Aortic or mitral IE with:
|
Urgent |
I |
B |
Aortic or mitral IE or severe prosthetic dehiscence with severe regurgitation and no heart failure |
Elective |
IIa |
B |
Right heart failure secondary to severe tricuspid regurgitation with poor response to diuretic therapy |
Urgent/ elective |
IIa |
C |
Uncontrolled Infection: Locally uncontrolled infection (abscess, false aneurysm, fistula, enlarging vegetation) |
Urgent |
I |
B |
Persisting fever and positive blood cultures for more than 7 to 10 days and not related to an extracardiac cause |
Urgent |
I |
B |
Infection caused by fungi or multiresistant organisms |
Urgent/ elective |
I |
B |
PVE caused by staphylococci or gram negative bacteria (most cases of early PVE) |
Urgent/ elective |
IIa |
C |
Prevention of Embolism: Aortic or mitral IE or PVE with large vegetations (>10 mm) following one or more embolic episodes despite appropriate antibiotic therapy |
Urgent |
I |
B |
Aortic or mitral IE or PVE with large vegetations (>10 mm) and other predictors of complicated course (heart failure, persistent infection, abscess) |
Urgent |
I |
C |
Aortic or mitral or PVE with isolated very large vegetations (>15 mm) |
Urgent |
Ib |
C |
Persistent tricuspid valve vegetations >20 mm after recurrent PE |
Urgent/ elective |
IIa |
C |