VALVE PROSTHESIS
MECHANICAL PROSTHESIS
- In use since 1960s
- Divided into caged-ball, disc (monodisc) and bileaflet valves
Caged-Ball Valves
|
Caged-Ball Valves Starr-Edwards valve
|
Disadvantage:
- Frequent thromboembolic complications
- Efforts to reduce this has led to development of the cloth-covered caged-ball valves
- Best valves were the Braunwald–Cutter valve and Cloth-covered Starr–Edwards valve
- Struts and the ring were covered with polypropylene into which endothelium grew within several weeks or months after implantation
- Thereby, except for the ball, blood did not contact a foreign surface
- Limited reduction in the incidence of thromboembolic events and haemolysis was achieved but remained limited to the first months or few years after implantation.
- Tearing of the cloth covering occurred as a result of hardness and disparity between the ball and the endothelialized covering
- This initiated thrombus formation with subsequent thromboembolic events
- Also caused clinically significant haemolysis
- All prompted reoperation and valve reimplantation
|
Caged-Ball Valves Cloth-covered Starr–Edwards valve
Caged-Ball Valves
Cloth-covered Braunwald–Cutter valve
|
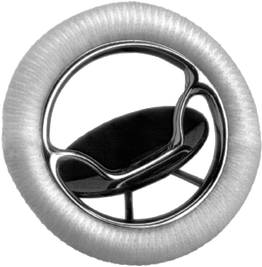
Disc Valves
Can be divided into Non-tilting and Tilting Disc valves
Non-Tilting Disc Valves
Can be divided into Non-tilting and Tilting Disc valves
Non-Tilting Disc Valves
- Non-tilting disc valves were introduced into clinical practice in the late 1960s into clinical practice.
- The closing component was a poppet that was held in a cage (open position) or obturated the ring (closed position)
- Best known valves:
Advantage:
Disadvantage:
- Low profile design
- Easier implantation
- Very little opening resistance
- Very short closure delay (hence very little regurgitation)
Disadvantage:
- Higher flow resistance
- Significant turbulence
- Frequent thromboembolic complications
- Higher haemolysis rate
Tilting Disc Valves
- Were the most-often implanted valves in the 1970s and 1980s.
- Precise knowledge of the tilting angle in monodisc and bileaflet valves is important for eventual diagnostics of the valve failure.
- Discs are radio-opaque and therefore fluoroscopy imaging can confirm their normal mobility or diagnose restricted range of motion, or even complete occluder blockade.
Disc valve Björk–Shiley
Standard type with at disc:
Standard type with at disc:
- The most commonly used valves In Europe .
- The First Model had a delrin disc, tilted up to 60°.
- Soon replaced by a the standard type with pyrolytic carbon at disc tilting up to 60°.
- Introduced in 1976.
- Has a significantly improved haemodynamics.
- Discontinued in the late 1980s because the inflow bar broke in some after 2–3 years of perfect performance, causing escape of the disc and acute valve regurgitation (can be lethal).
- Since then, the struts in all heart valves are not welded but manufactured from a single block of metal or alloy or from pyrolytic carbon.
- The latest Model.
- Introduced into clinical practice in 1982.
- The disc-housing system was changed and the angle of tilting was increased to 70°.
The Ultracor–Aortech valves (developed in 1985), the tilting angle of which is 73° in the aortic model and 68° in the mitral model, have also been implanted.
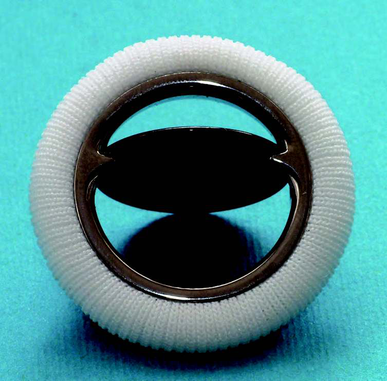
Bileaflet Valves
Gained popularity since the mid-1980s
Currently are the most frequently implanted valves in the world
Different types but all based on the same or similar principle but differ in:
Gained popularity since the mid-1980s
Currently are the most frequently implanted valves in the world
Different types but all based on the same or similar principle but differ in:
- Angle of tilting.
- Design of the pivots.
- Material and shape of the sewing ring.
- Depth of the leaflets in their open position.
St Jude Medical (SJM) valve:
SJM HP EOA = 2.03cm2
SJM Regent EOA = , 2.47cm2
- Best-known and most implanted mechanical bileaflet valve.
- In clinical practice in 1977 (SJM Standard).
- Semilunar leaflets open up to 85° and close at 30°, yielding a tilting range of 55°.
- SJM HP (hemodynamic plus, since 1992) and SJM Regent (since 1998) with a reduced sewing ring, which results in significant enlargement of the effective orifice area (EOA) (avoiding patient-prosthesis mismatch - PPM)
- EOA for Size 21-mm SJM is:
SJM HP EOA = 2.03cm2
SJM Regent EOA = , 2.47cm2
- SJM Regent 19-mm valve has an EOA of 1.84cm2 which is sufficient to prevent PPM in a patient with a body-surface area of 2cm2.
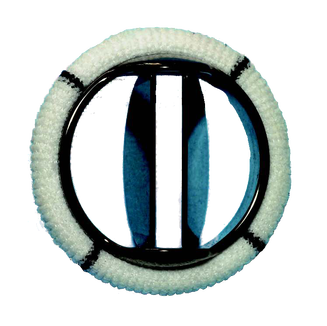
Bileaflet Bicarbon–Sorin
- Second most commonly implanted bileaflet valve.
- Manufactured since 1990.
- Semilunar leaflets are convex–concave shaped and tilt up to 80° and close at 20° .
- Sewing rings Fitline or Slimline (suitable for small annuli).
- Overline (intended solely for supra-annular implantation).
- The same mechanism, but a different sewing cuff material, is typical for the Edwards MIRA valve (since 1997).
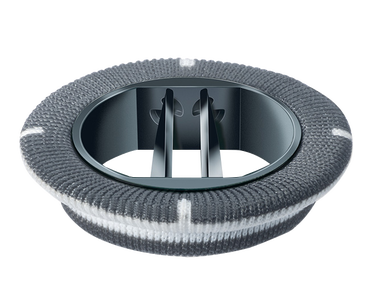
CarboMedics Valves
- In clinical use since 1986.
- Semilunar leaflets tilt up to 78° and close at 25°, which gives a tilting range of 53°.
|
CARBOMEDICS OPTIFORM: Adaptable for:
CARBOMEDICS R (Reduced)
|
- Medtronic Advantage has, since 2003, A modification for supra-annular implantation named Medtronic Advantage Supra.
- The most recent bileaflet valve introduced into clinical practice is the valve CardiaMed.
oN X VALVE
On-X Life Technologies, Austin, TX
- Bileaflet valve
- Constructed completely from pyrolytic carbon.
- Lack of silicon doping in the carbon construction potentially decreases its thrombogenicity.
- Has a tall flared inlet that increases the orifice area and decreases the ability of retained valve tissue to interfere with the opening and closing mechanisms.
- Has a stasis free pivot that allow the valve to wash out itself.
- Has a 90-degree leaflet opening which provides improved laminar flow and reduce turbulence.
- Available is three different sewing rings:
- Standard:
- Aortic: sizes from 19 to 27/29 mm
- Mitral: sizes from 23 to 31/33 mm.
- Conform X: has a more flexible sewing ring.
- Aortic: sizes from 19 to 27/29 mm.
- Mitral: only one size that fits an annular size ranging from 25 to 33 mm.
- Anatomic:
- Designed to for the contours of the aortic valve annulus.
- Sizes from 19 to 27/29 mm.
- Standard:
- PROACT Trial ( Prospective Randomised On-X Anticoagulation Clinical Trial)
- Compared low dose Warfarin plus low dose aspirin (81mg) to standard warfarin.
- The first showed a significantly lower major and minor bleeding rates.
- The incidence of stroke, TIA, total neurologic events and all cause mortality were similar