CORONARY ANGIOGRAPHY
INTODUCTION
- An invasive method to identify and quantify coronary artery disease (CAD):
– vessel dominance
– vascular territories
– anomalous vessels
– coronary collateral circulation
2. Coronary luminal obstruction: – guide revascularization decisions
- Severity of luminal narrowing
- Distribution of stenotic lesions
- Identification of acute, thrombotic lesions
3. Coronary blood flow
4. LV systolic and diastolic function, ejection fraction and regional wall motion
- The first attempts to visualize the coronary arteries in living humans were published in 1945 by Radner S who used trans-sternal punctures to inject contrast material into the ascending aorta. High complication rate with poor results, the technique was abandoned.
- The first selective coronary angiogram was performed by Mason Sones in 1959 through the brachial cut-down technique.
- With the prior introduction of the Seldinger wire cannulation method for vascular cannulation percutaneous transfemoral catheterization technique was developed.
- Judkins, Amplatz, Abrams and others invented preformed catheters that could be passed with great ease from the femoral artery to the coronary ostium.
- Arterial access: most commonly femoral; brachial or radial arteries can also be used
- Catheter size depends on several patient variables including:
2. Aortic valve plane orientation
3. Angle of coronary ostial origin
- Typically, left and right Judkins catheters are used to engage the left coronary artery (LCA) and the right coronary artery (RCA) respectively
- Provides excellent delineation of coronary anatomy in vessels > 400um in diameter.
- Mainly shows the anatomy of the arterial lumen opposed to the wall of the artery.
- It is a 2D shadow of a 3D object.
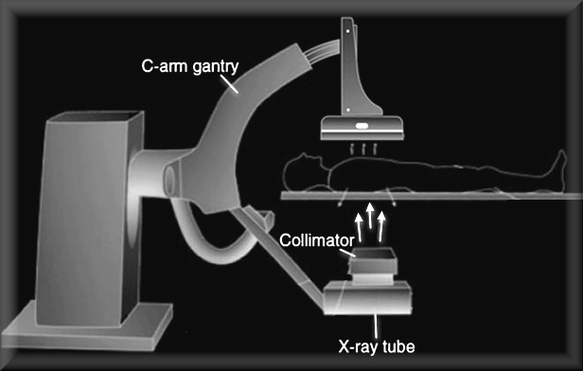
Schematic of radiographic imaging system
The X-rey beam is generated by an X-ray tube. The beam passes through a collimator where lead apratures form and limit the beam. On intersection with the patient, most of the beam is reflected or absorbed. The remaining photons pass through the image intensifier.
Thirty to sixty exposures are needed to give appearance of a Live continuous image
The X-rey beam is generated by an X-ray tube. The beam passes through a collimator where lead apratures form and limit the beam. On intersection with the patient, most of the beam is reflected or absorbed. The remaining photons pass through the image intensifier.
Thirty to sixty exposures are needed to give appearance of a Live continuous image
INDICATIONS
- Acute STEMI to identify and reperfuse the infarct-related artery
- Acute STEMI who have received lytic or medical therapy and have - recurrent angina - heart failure - Arrhythmia or for risk stratification purposes
- NSTEMI or Unstable Angina in whom an invasive management strategy is chosen
- Evaluation of select stable angina patients with or without a prior, abnormal noninvasive test
- Evaluation of certain ‘high-risk’ asymptomatic patients
- Patients with chest pain syndromes and abnormal or nondiagnostic noninvasive tests
- Pre-operative evaluation for select patients undergoing non-cardiac surgery
- Pre-operative evaluation for select patients undergoing cardiac surgery
- Evaluation of heart failure syndromes to exclude significant coronary disease
- Other conditions (hypertrophic obstructive cardiomyopathy, aortic dissection, chest trauma)
CONTRAINDICATIONS
- Patients who do not desire or who are not candidates for revascularization
- Patients in whom revascularization is unlikely to improve quality/duration of life
- As a screening test for CAD in asymptomatic patients
- Routine angiography within 24 hours of lytic therapy in the absence of ongoing ischemia
- Acute renal failure, marked electrolyte imbalance, or metabolic disarray
- Active bleeding or severe coagulopathy
- Prior cholesterol embolization syndrome or anaphylaxis to contrast
- Active infection or unexplained fever
- Decompensated respiratory status, heart failure, or uncontrolled hypertension
- Changing mental status or inability to cooperate
COMPLICATIONS
Coronary arteriography is generally a safe procedure.
The overall incidence of complications and mortality increases directly with:
– ST/T wave changes
– Allergic reaction (urticaria, bronchospasm, angioedema, laryngospasm, anaphylaxis)
The overall incidence of complications and mortality increases directly with:
- Extent of coronary artery disease, particularly left main coronary stenosis
- Presence of coexistent significant valvular disease
- Reduced ventricular ejection fraction
- Reduced functional state
- Advancing age
- Arrhythmia
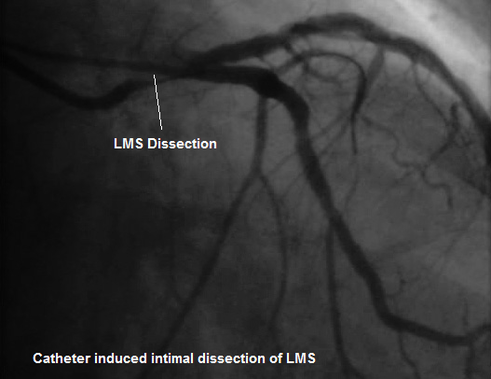
- Coronary artery dissection or embolization
- Myocardial infarction
- Heart failure
- Death
- Stroke
- Contrast toxicity/reaction:
– ST/T wave changes
– Allergic reaction (urticaria, bronchospasm, angioedema, laryngospasm, anaphylaxis)
- Renal failure
- Vascular complications: hematoma, AV fistula, pseudo-aneurysm
- Neurologic:
- Local femoral or brachial artery injury from arterial cannulation and compression for haemostasis
- Ulnar nerve compression from prolonged procedures
- Transient Ischaemic Attacks and Strokes: mostly embolic from the aorta
CATHETER INDUCED TRAUMA
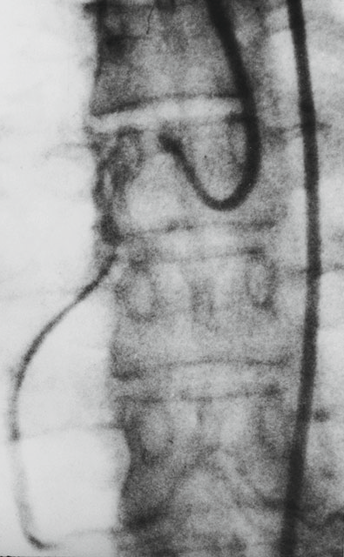
EMBOLIZATION
|
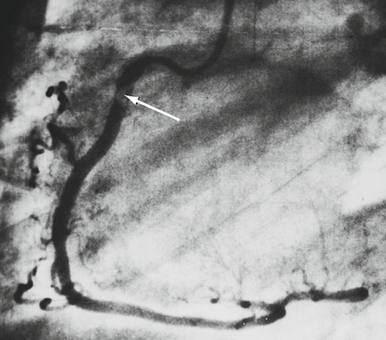
LAO view of RC arteriogram
Evidence of embolic material probably from a catheter thrombus, or less likely, from an atherosclerotic plaque; large RCA. Filling defect ( arrow ) can be seen clearly and was observed to migrate toward the periphery |
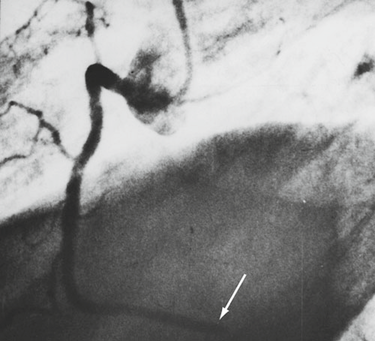
LAO view of RC arteriogram
Repeat injection now shows occlusion ( arrow ) of the PDA |