AORTIC VALVE STENOSIS
INDICATION FOR SURGERY
In the decision making of AVR, the following should be taken into consideration:
- Clinical status: symptomatic or asymptomatic.
- Severity of the aortic stenosis.
- Isolated aortic valve procedure versus combined procedure.
- Left ventricular function and dimensions.
- Comorbidities.
2014 ACC/AHA Guidelines for AVR in Aortic Stenosis*
The guidelines classify progression of AS into 4 stages (A to D):
Classification of progression of AS |
Stage A: At risk of AS (Bicuspid, Congenital, or Valve Sclerosis). |
Stage B: Progressive AS (Mild to Moderate Severity). |
Stage C: Asymptomatic severe AS, as follows:
|
Stage D: Symptomatic severe AS:
|
RECOMMENDATION |
CLASS |
LEVEL |
AVR is recommended for severe high-gradient symptomatic AS (by history or on exercise testing) (stage D1) |
I |
B |
AVR is recommended for asymptomatic severe AS (stage C2) and LVEF < 50% |
I |
B |
AVR is indicated for severe AS (stage C or D) undergoing other cardiac surgery |
I |
B |
AVR is reasonable in asymptomatic very severe AS (stage C1, Jet velocity ≥ 5.0 m/s) and low surgical risk |
IIa |
B |
AVR is reasonable in asymptomatic (stage C1) severe AS and decreased ET or an exercise fall in BP |
IIa |
B |
AVR is reasonable in symptomatic low-flow/low-gradient severe AS with reduced LVEF (stage D2) with a low-dose DSE that shows: jet velocity ≥ 4.0 m/s or mean gradient ≥ 40 mm Hg with a AVA ≤ 1.0 cm² at any dobutamine dose |
IIa |
B |
AVR is reasonable in symptomatic low-flow/low-gradient severe AS (stage D3) in normotensive and LVEF ≥ 50% (if clinical, hemodynamic, and anatomic data support valve obstruction as the most likely cause of symptoms) |
IIa |
C |
AVR is reasonable in moderate AS (stage B) (jet velocity 3.0 to 3.9 m/s) undergoing other cardiac surgery |
IIa |
C |
AVR may be considered for asymptomatic severe AS (stage C1) and rapid disease progression and low surgical risk |
IIb |
C |
Assessment of Severity:
The severity can be assessed by either echocardiography or cardiac catheterization.
Echocardiography:
The severity can be assessed by either echocardiography or cardiac catheterization.
Echocardiography:
- The Diagnostic Tool of Choice in diagnosis and quantification of severity.
- Can defines the severity and aetiology of AS.
- Defines any coexisting valvular abnormalities.
- Defines cardiac chamber size and function.
- Measures the maximum jet velocity and the mean transvalvular gradient.
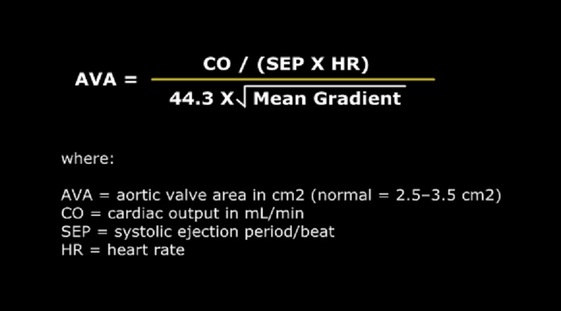
- Calculation of the AVA using the continuity equation.
- Can also measure the valve area directly by planimetry in the short-axis view.
- Quantification of diastolic dysfunction by measures LV filling pressures.
- LV Filling Pressures: calculating the ratio of trans-mitral flow velocity and annular velocity using tissue doppler at the level of the mitral annulus by
Correlation of Echocardiographic Measurements with the
Severity of Aortic Valve
Severity of Aortic Valve
Indicator |
Mild |
Moderate |
Severe |
Jet Velocity |
< 3.0 |
3.0-4.0 |
> 4.0 |
Mean Gradient (mm Hg) |
< 25 |
25 - 40 |
> 40 |
Aortic Valve Area (AVA) (cm²) |
> 1.5 |
1.0 - 1.5 |
< 1.0 |
Aortic Valve Area Index (cm²/m²) |
< 0.6 |
||
Dimensionless Index |
< 25 |
Gradients are significantly influenced by the cardiac output and therefore the aortic valve orifice area should be taken into consideration in preference.
Management strategy for patients with severe aortic stenosis
Cardiac Catheterization:
- By measuring the transvalvular flow (the cardiac output or stroke volume).
- Calculation of the peak or mean pressure gradient across the valve: from pressures obtained on a catheter pull-back from the left ventricle into the aorta.
- Valve area is calculated using the Gorlin formula:
- Low gradients may be noted in low cardiac output states despite severe AS.
- High gradients may be noted in high output states in the absence of severe AS.
- This may cause apparent inconsistencies in the degree of AS using different measurements and in different clinical states.
- Critically narrowed valve may not be possible to be crossed with a catheter. Here, echocardiography should be sufficient.
- Due to the increased risk of embolic stroke, hemodynamic assessment of AS during catheterization is not recommended (a class III recommendation) unless echo results are equivocal.
- Coronary angiography is indicated before surgery to identify whether CAD is present.
Surgery for Asymptomatic Aortic Valve Stenosis *
Note: Stress testing is contraindicated in the symptomatic patient with severe AS.
ii. Severe AS with high likelihood of progression (elderly patients, calcified valve, presence of
CAD) or if there will be a potential delay from symptom onset to surgery.
Estimated rate of progression:
- Reduction of AVA by 0.14cm2 per Year.
- Increase in the mean gradient by 7 mmHg per year.
iii. Critical AS (AVA<0.6 cm2, mean gradient>60mmHg, jet velocity>5.0 m/s).
- Surgery is not traditionally considered for the asymptomatic patient, regardless the degree of stenosis, because the risk of sudden death is considered to be low (estimated at<1%/year), and the risk of the AVR may exceed the potential benefit of surgery.
- Severe AS need to be followed carefully for the development of symptoms or rapidly progressive valve stenosis.
- Failure to perform surgery once patients become symptomatic is the most important risk factor for late mortality.
- up to 40% of patients with severe AS will become symptomatic within 2 years.
- About 67% will be symptomatic by 5 years.
- Rate of progression of AS is faster and the symptom free interval is shorter in:
- Stenotic valve with high jet velocities.
- Presence of LV hypertrophy.
- Presence of severe valve calcification.
- Class I: LV systolic dysfunction (EF<50%).
- Class IIb:
Note: Stress testing is contraindicated in the symptomatic patient with severe AS.
ii. Severe AS with high likelihood of progression (elderly patients, calcified valve, presence of
CAD) or if there will be a potential delay from symptom onset to surgery.
Estimated rate of progression:
- Reduction of AVA by 0.14cm2 per Year.
- Increase in the mean gradient by 7 mmHg per year.
iii. Critical AS (AVA<0.6 cm2, mean gradient>60mmHg, jet velocity>5.0 m/s).
- Asymptomatic moderate AS (AVA < 1.2 - 1.4 cm2, mean gradient 25-40 mmHg, Vmax 3-4m/s) with concomitant cardiac surgery (higher risk of reoperative surgery).
- Planed major non cardiac surgery.
- Planned pregnancy.
Symptomatic Severe Aortic Stenosis
- Symptomatic severe aortic stenosis is a straightforward indication for surgery.
- Once symptoms are present, the average survival is about 2 years
- Less than 20% chance of surviving 5 years.
- Mean survival is:
- 1 year for patients with CHF.
- 2 years with syncope.
- 4 years with angina.
- 1 year for patients with CHF.
- Myocardial Contractile Reserve has to be tested, usually by dobutamine stress echocardiography in symptomatic severe aortic stenosis with low EF (<35%) and low mean gradient (<30mmHg).
Dobutamine Stress Echocardiography (DSE)
- Assess the severity of AS with a low gradient (mean gradient <30mmHg) and poor LV (EF <35%).
- The calculated valve area may be consistent with severe AS, although the degree of AS may not be significant.
- DSE can be used to determine whether poor LV with a low stroke volume is primarily related to afterload mismatch from true severe AS or is secondary to contractile dysfunction.
- An increase in stroke volume and cardiac output with little increase in gradient, the AVA will increase, indicating overestimated severity of AS and surgery is not indicated.
- An increase in the EF (>10%) stroke volume (>20%) and the gradient (>30%), the AVA will remain the same, confirming a true AS that will benefit from surgery.
- Failure to produce an increase in stroke volume, confirms poor contractile reserve (<20% increase in stroke volume with DSE) and is a high risk for surgery; Some argue that surgery would still have a better long-term prognosis than with medical management. Alternatively TAVI approach may be preferable in this situation.
- Young age, large annulus, absence of comorbidities, may facilitate the decision to replace the aortic valve; otherwise, heart transplantation is the only solution.
- Mechanical ventricular assistance devices as a bridge to transplant.
- Studies suggest an elevated B-type Natriuretic Peptide (BNP) level (>550) is a very strong predictor of operative mortality, even more important than contractile reserve measured by DSE.
Associated Ascending Aorta Dilatation:
- When indications for aortic valve surgery are met and an enlarged aorta 4.5 cm is present, the ascending aorta should also be replaced.
- Although this is a standard criterion for bicuspid valves, it is not inappropriate for patients with trileaflet valves.
* Based on 2014 ACC/AHA Guidelines (http://www.cardiosource.org/)